Maternal data collection
This page contains information about how women's deaths, occurring during pregnancy or in the year after the end of pregnancy, are identified, and how MBRRACE-UK collects these data.
For guidance on how to notify MBRRACE-UK of a maternal death, please Contact Us.
Identification of maternal deaths
MBRRACE-UK records and collects information on all women who die in the UK (or the Republic of Ireland) during pregnancy or up to one year after the end of pregnancy regardless of how the pregnancy ends and the place and circumstances of the death.
The majority of women's deaths are notified directly to the MBRRACE-UK office at the University of Oxford by the trust/health board where the woman gave birth or where the death occurred. Each trust/health board in the UK that provides maternity care should have nominated staff members who are responsible for reporting maternal deaths. The MBRRACE-UK office at the University of Oxford should be notified within one week of the death occurring, or of becoming aware of the death.
Please note that anyone can report a maternal death. In some instances, the responsibility may not be on the trust/health board where the woman gave birth or died, but instead on whomever is first to become aware of the death. In some instances deaths may be identified through other sources including coroners or procurator fiscals, pathologists, Local Supervising Authority Midwifery Officers and members of the public or media.
Note: Trusts in England are now required to report maternal deaths through the Submit a Perinatal Event Notification (SPEN) portal. This change does not impact Health Boards in Northern Ireland, Scotland or Wales and does not change the eligibility, reporting requirements or deadlines for notification.
To ensure that all relevant deaths are captured by MBRRACE-UK, data held by MBRRACE-UK are checked against national death and birth registries from the Office of National Statistics (ONS) and National Records of Scotland (NRS). These sources provide details on deaths where pregnancy or a pregnancy-specific cause of death is noted on the death registration. Data linkages between these sources also help identify women of reproductive age who died in the year following birth who don't have a pregnancy or pregnancy-specific cause of death noted on the death registration. In this way, MBRRACE-UK is able to a) confirm that a woman has died and b) identify any women who died who may have been missed through standard reporting procedures.
Collecting and reporting surveillance information
Data collection
MBRRACE-UK collects comprehensive surveillance data for every woman who dies during pregnancy or up to one year after pregnancy in the UK. These data include women's sociodemographic characteristics, information on her health, medical and pregnancy history, and details about the woman's birth and the cause of her death. Collection of these data allows MBRRACE-UK to examine the risk factors for maternal mortality in the UK and gain a clearer understanding of the health, social and lifestyle factors most often linked to maternal deaths.
All information collected by MBRRACE-UK is entered into a secure, bespoke database and entries are double checked by a member of the MBRRACE-UK team. Any queries about missing or unclear data entries are sent back to the units or taken from the woman's records to ensure that the data are of high quality.
Data reporting
MBRRACE-UK collects information about all women who die in the UK during pregnancy and up to one year after pregnancy regardless of how she died, the duration of her pregnancy or how her pregnancy ended. However, to align with international reporting, the majority of data reported by MBRRACE-UK includes only women who died during or up to six weeks after pregnancy from causes directly related to pregnancy (direct maternal deaths) or affected by pregnancy (indirect maternal deaths).
Definitions of maternal deaths
Maternal death: The death of a woman while pregnant or within six weeks after the end of pregnancy, from causes related to pregnancy or made worse by it, regardless of how long the pregnancy was or how it ended (birth, miscarriage, termination, or ectopic pregnancy).
Direct maternal death: The death of a woman resulting from complications of pregnancy, childbirth or the management of pregnancy including interventions or treatment. Examples include deaths due to bleeding, blood clots, suicide and pre-eclampsia.
Indirect maternal death: The death of a woman due to a medical condition or disease that the woman had before pregnancy or developed during pregnancy. The condition or disease was not the direct result of pregnancy but may have been made worse by the physical changes of pregnancy. Examples include deaths due to heart disease and epilepsy.
Coincidental maternal death: The death of a woman from a cause completely unrelated to pregnancy that happened to occur while the woman was pregnant or recently pregnant. Examples include road traffic accidents and homicides.
Late maternal death: The death of a woman, from any cause, which occurs between six weeks and one year after the end of pregnancy, regardless of how long the pregnancy was or how it ended (birth, miscarriage, termination, or ectopic pregnancy).
Maternal mortality rates
Since maternal deaths in the UK are rare, MBRRACE-UK reporting combines three years' worth of data to identify meaningful trends. Rates for the devolved nations are typically not reported alongside UK-wide maternal mortality rates because small numbers in some devolved nations mean that these figures are subject to significant variation, which make comparisons unreliable.
Maternal mortality rates are calculated by dividing the number of deaths by the number of maternities (the denominator) in a given three-year period. The number of maternities includes all women giving birth in the UK, including both live births and stillbirths. This differs from standard international maternal mortality ratios that use live births as the denominator. The number of maternities are obtained from the annually reported birth data for England and Wales (Office for National Statistics), Scotland (General Register Office for Scotland) and Northern Ireland (Northern Ireland Statistics and Research Agency).
Maternal mortality rates are presented as the number of deaths per 100,000 maternities with 95% confidence intervals.
Several maternal mortality rates are presented by MBRRACE-UK:
- Overall maternal mortality rate: includes women who died in the UK during pregnancy or up to six weeks after pregnancy from direct and indirect causes of death
- Direct maternal mortality rate: includes women who died in the UK during pregnancy or up to six weeks after pregnancy from direct causes of death
- Indirect maternal mortality rate: includes women who died in the UK during pregnancy or up to six weeks after pregnancy from indirect causes of death
- Cause-specific maternal mortality rate: includes women who died in the UK during pregnancy or up to six weeks after pregnancy from a specific cause of death
- Late maternal mortality rate: includes women who died in the UK between six weeks and one year after the end of pregnancy from any cause of death
Maternal mortality rates are also reported for specific populations including women belonging to different age groups, women from different ethnic backgrounds and women living in different areas of deprivation.
Reporting by ethnic group
Women's ethnicity is collected as part of MBRRACE-UK surveillance data. Ethnic categories used are those in the ONS 2001 Census
Since there may be very few women who die who belong to specific ethnic groups, the ethnicity data collected as part of MBRRACE-UK surveillance are re-grouped to allow for better comparisons. Maternal ethnicity data are re-categorised in two ways and reported on as follows:
- The proportion of the women who died in the UK, grouped by eight ethnic categories: White European, Indian, Pakistani, Bangladeshi, Other Asian (including Chinese), Black Caribbean, Black African and Others/Mixed
- The maternal mortality rate for women who died in England, grouped by five ethnic categories: White (including women whose ethnicity is not known), Asian, Black, Chinese/Other and Mixed
The maternal mortality rates for different ethnic groups are calculated by dividing the number of deaths by the number of maternities (the denominator) in each ethnic group. The number of maternities for each ethnic group is obtained from the annually reported NHS Maternity Statistics for England, which includes data on deliveries taken from Hospital Episode Statistics (HES). The ethnic categories used to calculate maternal mortality rates are the same as those used by Hospital Episode Statistics (HES).
Maternal mortality rates for different ethnic groups are presented as the number of deaths per 100,000 maternities with 95% confidence intervals. The maternal mortality rates for women from Black, Asian, Chinese/Other and Mixed ethnic backgrounds are compared to maternal mortality rates for White women. This comparison generates a rate ratio (or relative risk) that is presented with 95% confidence intervals. The rate ratio represents the risk of maternal death for women in each ethnic group compared to White women (the reference group).
Reporting by deprivation
Postcodes are collected for all women whose deaths are reported to MBRRACE-UK. This information helps show the level of deprivation in the area where the woman lived.
In England, small areas of the country are ranked from most deprived to least deprived using government statistics called the Index of Multiple Deprivation (IMD). For women who die in England, their postcodes are mapped to these small areas to produce a deprivation score based on where they live. This score is used to group women into five different IMD categories (quintiles). Quintiles are used instead of deciles (10 different categories) so there are enough women in each group to make meaningful comparisons. For MBRRACE-UK reporting, IMD I represents the least deprived group and IMD V the most deprived.
The maternal mortality rates for different IMD quintiles are calculated by dividing the number of deaths by the number of maternities (the denominator) in each quintile. The number of maternities for each IMD quintile is obtained from the annually reported NHS Maternity Statistics for England, which includes data on deliveries taken from Hospital Episode Statistics (HES). Since Hospital Episode Statistics (HES) data are presented by decile, not quintile, the number of maternities in two consecutive deciles are added together to produce the denominator figure for each quintile.
Maternal mortality rates for woman's level of deprivation are presented as the number of deaths per 100,000 maternities with 95% confidence intervals. The maternal mortality rates for women from IMD II, IMD III, IMD IV and IMD V (most deprived) are compared to maternal mortality rates for women from IMD I (least deprived). This comparison generates a rate ratio (or relative risk) that is presented with 95% confidence intervals. The rate ratio represents the risk of maternal death for women living in more deprived areas compared to women living in the least deprived areaas (the reference group).
Reporting small numbers
To avoid revealing information that could potentially identify individuals, maternal mortality rates based on a very small number of deaths (<3 in any category) are not reported.
Collecting information for confidential enquiries
For all women who die during pregnancy or up to a year after pregnancy in the UK and Ireland, MBRRACE-UK requests and collects:
- Hospital records from all units that were involved in the woman's care from one year prior to pregnancy to her death. The hospital records collected include, but are not limited to, maternity notes, critical care or ICU records, and A&E notes.
- GP records from GPs involved in the woman's care from one year prior to pregnancy to her death.
- Records from relevant ambulance trusts/services including patient records, 999 call logs and transcripts, documented communications, and reviews (including quality assessments)
- A copy of the woman's post-mortem report if one has been undertaken. These help ensure that the woman's cause of death is accurate.
- Local clinician reports (LCRs) completed by key individuals involved in the woman's care. These confidential reports describe local factors impacting on women's deaths and any lessons to be learned.
- Copies of any relevant local hospital reviews and investigations including those conducted by the Maternity and Newborn Safety Investigations (MNSI) programme.
Where applicable to the woman's care, MBRRACE-UK also requests notes from other agencies or specialist services, such those caring for women with mental health problems, cancer, or neurological conditions like epilepsy.
Hospital, ambulance and GP records are also requested for women who did not die but who experienced severe morbidity during pregnancy and are included in annual topic-specific morbidity confidential enquiries. For these women, the notes are requested from one year prior to pregnancy up to six weeks after the end of pregnancy.
All information collected by MBRRACE-UK is fully anonymised before it is uploaded to a secure online platform. These documents are then reviewed by MBRRACE-UK assessors as part of the confidential enquiry process.
Identifying and collecting information about maternal deaths in Northern Ireland
All maternal deaths occurring in Northern Ireland are reported to MBRRACE-UK, however, privacy issues in Northern Ireland restrict identifiable information from being transferred out of the province. As such, all maternal deaths are reported to staff at the Northern Ireland Maternal and Child Health (NIMACH) office of the Public Health Agency of Northern Ireland. Surveillance data and case notes are then fully anonymised before being securely transferred to the MBRRACE-UK office at the University of Oxford.
Identifying and collecting information about maternal deaths in the Republic of Ireland
MBRRACE-UK also collects information on the deaths of all women during or up to a year after the end of pregnancy that occur in the Republic of Ireland. These deaths are not included in MBRRACE-UK's routine surveillance data and do not contribute to the UK's maternal mortality rates but they are included in MBRRACE-UK's confidential enquiries. As there are very few maternal deaths in Ireland, reviewing them alongside UK deaths helps maintain confidentiality and anonymity.
As with Northern Ireland, maternal deaths occurring in the Republic of Ireland are not reported directly to MBRRACE-UK. Instead, these deaths are identified by The Maternal Death Enquiry (MDE) Ireland and all information is fully anonymised before being sent to the MBRRACE-UK office.
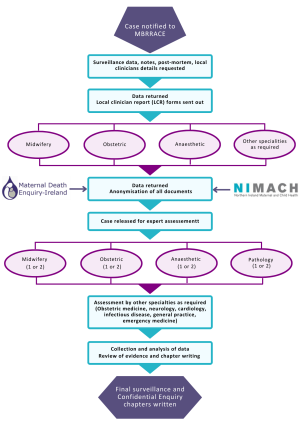
The data collection and review (flow diagram)